Appendicitis – Underdiagnosed in Rabbits?
Clinical Connections – Autumn 2024
Joanna Hedley, Senior Lecturer in Exotic Species and Small Mammal Medicine and Surgery
‘Gut stasis’ or ‘gastrointestinal syndrome’ is one of the most common reasons for rabbits to be presented to the RVC Exotics Referral Service.

While a rabbit with uncomplicated gut stasis can usually be managed symptomatically in first opinion practice, many of the cases we see are more critical patients, often requiring intensive care in hospital with us.
We also see patients who are having recurrent bouts of stasis with no obvious trigger.
The initial approach to any rabbit with gut stasis always starts with stabilisation, often including active warming, intravenous fluid therapy, nutritional support, analgesia and prokinetics as required. Once treatment has been initiated, the focus can then move onto identifying the underlying cause.
Diagnostic approaches
The diagnostic approach will depend on whether the signs are thought to be primarily due to gastrointestinal disease or secondary to pain elsewhere, stress or systemic disease.
Bloodwork, full dental examination under sedation and initial imaging – such as radiography – can be easily performed in-house. However in many of the more challenging cases, we have found advanced imaging to be increasingly helpful, specifically to identify any focus of pain or structural abnormality, which may be resulting in the gut stasis signs.
Dental changes, arthritis and spondylosis are common causes of pain which may be diagnosed with radiography once changes are moderate-advanced, but often appreciated at a much earlier stage on CT scan.
Once underlying causes like these are identified and treated, gut stasis episodes can often be resolved. However the more CT scans performed in these cases, the more we are finding not just these common causes of gut stasis but also some unexpected findings.
Important differential
In recent years, appendicitis with associated sacculitis has been recognised as an important differential for gut stasis +/- abdominal pain, inappetence and weight loss in rabbits.
As a prey species, the presence and degree of pain in rabbits can be hard to assess, as they will naturally hide any signs of weakness from us, the predator species. Appendicitis cases can, therefore, often be chronic with rabbits just presenting with a prolonged non-resolving gut stasis episode or recurrent signs, despite standard supportive treatment.
Some cases provide more obvious clues, such as pyrexia or haematological changes, but this is not always the case. In fact, some cases may actually present hypothermic instead and co-morbidities are not uncommon, which can confuse diagnosis.
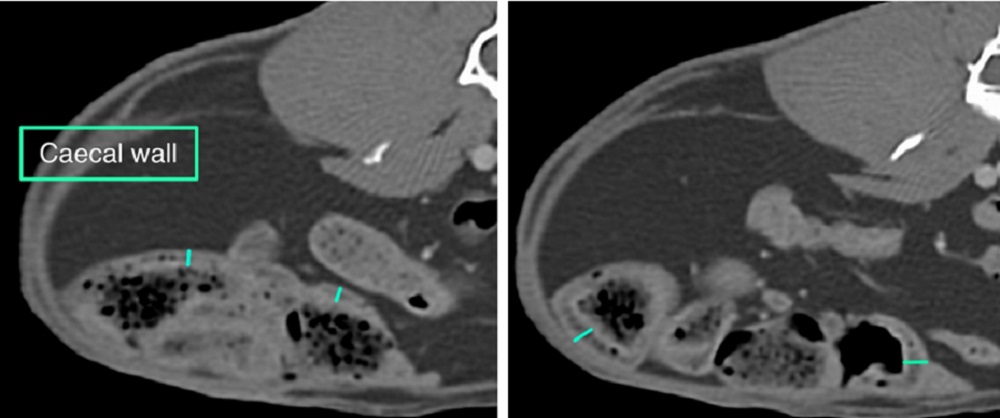
While changes in the appendix and sacculus rotundus may be visualised on abdominal ultrasound, the amount of gas present in rabbits with gut stasis may limit definitive diagnosis in some cases. This is where we find CT scans to be an invaluable diagnostic tool, as dilation of the appendix and thickening of the sacculus rotundus can be quickly visualised, allowing speedy treatment.
In the literature, a mix of medical and surgical treatment is described and surgical treatment has been suggested to carry a better prognosis. However the majority of cases that we have seen have been rabbits with recurrent gut stasis episodes, rather than critical cases requiring appendectomy.
These more chronic cases, in our experience, have responded extremely well to medical treatment with antibiotics, in addition to the normal supportive treatment given to our gut stasis patients.
We therefore strongly recommend considering appendicitis and sacculitis as a differential for these patients – and advanced imaging for diagnosis, when required, as it can make a real difference to resolving these more challenging cases.
