Rare Vascular Malformation of the Caudal Vena Cava
Clinical Connections – Summer 2022
A one-year-old Rottweiler was treated for an acquired traumatic kink in her caudal vena cava that was responsible for post-sinusoidal venous hypertension. The trauma was most likely caused by an altercation with a deer.
Lorna had a massive volume of fluid in her abdomen because of the caudal caval obstruction and this was refractory to medical treatment. Without some kind of intervention to manage the stricture, she had no future.
Having been initially seen by the RVC’s Emergency and Critical Care Service and the Cardiology Service, Lorna underwent surgical exploration of her caudal right hemithorax and excision of scar tissue surrounding the intrathoracic caudal vena cava. In addition, a patch of pericardium was sutured into the caudal vena cava across the area of greatest narrowing to increase the caudal caval diameter.
The surgery was performed by Dan Brockman, Professor of Small Animal Surgery and Director of the Cardiothoracic Surgery Service, supported in surgery by Carlos Alonso, our third-year surgery resident and Nuria Quesada Vicent, our third-year anaesthesia resident.
Lorna was referred to the Emergency and Critical Care Service early last May with ascites and suspected right-sided cardiac failure. On presentation she was bright and alert and was found to be cardiovascularly stable. Ultrasound confirmed the presence of fluid in her abdomen. Chest radiographs revealed rib fractures but no other abnormalities.
An echocardiogram revealed an abnormal structure at the base of her heart. Because of the unusual nature of this finding, multidisciplinary case conference with cardiology and surgery colleagues was held and the conclusion was that the lesion was either a rare congenital or acquired vascular malformation; and concluded a CT scan would be an invaluable additional investigation.
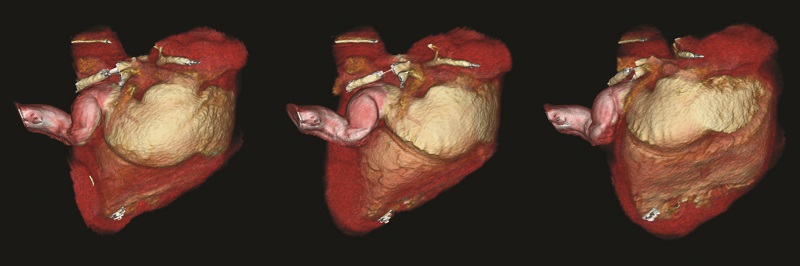
Lorna had CT of her thorax and abdomen on returning to the hospital on May 13th. At that point the combined cardiology and surgery teams were able to confirm that Lorna had an extremely rare malformation of her caudal vena cava, resulting in high pressure in her caudal vena cava (Budd-Chiari like syndrome), that was the cause of her ascites. Her heart was found to be otherwise normal in structure.
Lorna’s clinical presentation was comparable to other dogs reported in the veterinary literature describing kinking and tortuosity of the caudal vena cava. Previously documented dogs often presented in young adulthood following blunt thoracic trauma. Lorna's history of a possible altercation with a deer, and imaging evidence of rib fractures, mirrored these cases.
Possible treatments included surgical exploration and resection of the scar tissue causing obstruction, resection of the narrow part of the caudal cava and catheter-guided balloon dilation of the lesion with stent placement. No one on the RVC team had performed treatment on such a lesion but we suspected that balloon dilation and/or stenting would be a less appropriate option as the kinking of the vena cava was likely associated with fibrous tissue causing extra-luminal compression and there would be a high risk of recurrence of the stricture and we preferred to avoid an intravascular implant in such a young dog.
Lorna’s owners decided to go ahead with surgery, and she returned for admission on July 6th. Outlining the process, Professor Brockman said: “Because of the history of trauma and the high probability that Lorna had an acquired traumatic kink in her caudal vena cava that was responsible for the post-sinusoidal venous hypertension, we elected to explore the cava through a right sixth intercostal thoracotomy. At surgery, the scar tissue responsible for the ‘kink’ was very obvious and incorporated the right phrenic nerve, which was discontinuous.
“Having released the cava from the scar tissue, the caudal caval pressure remained slightly above cranial caval pressure, so a patch of pericardium was sutured into a longitudinal incision across the stricture, made in the caudal cava made inside a carefully positioned Satinsky clamp. This reduced the caudal caval pressure such that it was just above mean cranial caval pressure.”

Lorna recovered from surgery uneventfully and was discharged on antiplatelet drugs (aspirin and clopidogrel) for one month, to reduce the risk of clots forming on the pericardial patch. The owners were asked to go to the referring practice for staple removal and return to the RVC for check-up.
She returned for her check-up towards the end of August, prior to which she had been doing very well at home. On examination she was bright, alert and responsive. Her mucous membranes were pink and moist with a capillary refill time of under two seconds. Her heart rate was 92, with synchronous pulses. Her thoracic auscultation and abdominal palpation were unremarkable, with no evidence of a fluid thrill. Doppler echocardiography revealed a structurally normal heart, as before. there was no evidence of congestion of the abdominal aorta or hepatic veins and no ascites so strong evidence that caudal caval hypertension had been relieved. Lorna came 4th in her category at Crufts.
