Sentinel Lymph Node Mapping – Leading the Way in Veterinary Oncology
Clinical Connections – Summer 2023
Andy Yale, Lecturer in Veterinary Oncology
Cancer is a common disease in older cats and dogs but, as more advanced diagnostic and treatment modalities become available, the prognosis and quality of life of many pets with cancer can be good.
Sentinel lymph node (SLN) mapping is a diagnostic tool commonplace in human oncology and developing in veterinary oncology. It increases the accuracy of detection of metastatic disease whilst minimising patient morbidity.
With increased detection of metastasis, more patients can be offered additional therapies that may not have otherwise been considered – thus improving outcomes.
Cancer commonly spreads to lymph nodes (LNs) and, historically, assessment for LN spread would be based on cytology of LNs that are anatomically closest to the tumour, and/or regional LNs that are enlarged. However, there are limitations to this approach as tumours can develop unpredictable lymphatic drainage patterns – meaning they may drain to LNs distant to the tumour location, bypassing more local LNs.
Additionally, many normal-sized LNs can still harbour metastatic disease. Thoroughly assessing for LN metastasis without specific techniques, such as SLN, mapping would therefore involve sampling multiple LNs, with associated increased patient morbidity. It may also risk missing LN metastasis as LNs considered less likely to be draining the tumour, based on anatomic location, are unlikely to be sampled with this approach.
Sentinel LN mapping involves the administration of a contrast agent around the primary tumour or scar, followed by an imaging technique to visualise the exact LN(s) that drain the patient’s tumour. These ‘sentinel’ LNs are then sampled to check for metastasis.
This means LN sampling can be much more specific and personalised, both increasing the accuracy of metastasis detection and reducing patient morbidity. There are a variety of techniques available for SLN mapping, although CT and ultrasound-based techniques are most common in veterinary oncology.

Case study – Beetle
Beetle, a nine-year 11-month female neutered Labrador, was seen by RVC Small Animal Referrals’ Oncology Service in 2021. Beetle had an incompletely excised low-grade (Kiupel), intermediate-grade (Patnaik) mast cell tumour (MCT) on the head, situated midline above both eyes.
Despite being low- to intermediate-grade, the MCT had a high Ki67 index (>1.8%) – indicating a more aggressive biologic behaviour. Therefore, thorough staging prior to revision surgery and adjuvant chemotherapy was discussed.
Staging without techniques such as SLN mapping would have involved sampling many LNs as the lymphatic drainage patterns of head and oral tumours can be especially unpredictable. Lymph nodes targeted would have included bilateral mandibular, medial retropharyngeal, parotid and prescapular LNs (a total of eight, many of which require ultrasound-guided sampling).
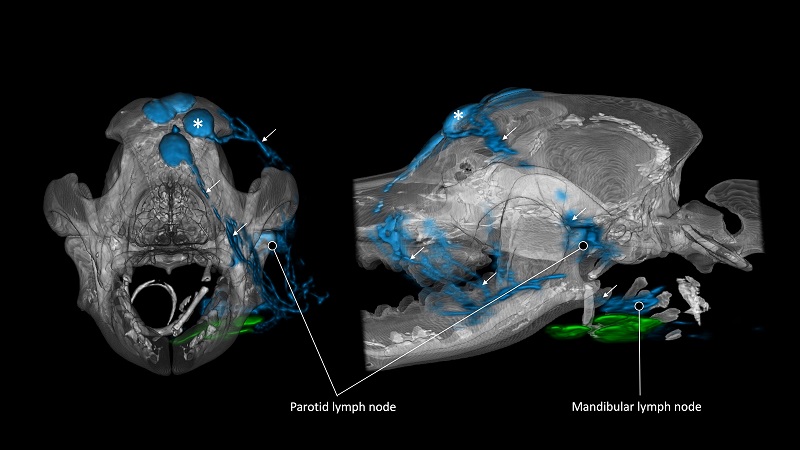
Following SLN mapping via indirect CT lymphography (ICTL), three SLNs were identified (left parotid LN, bilateral mandibular LNs). Cytology of these did not identify MCT metastasis but, as cytology can miss MCT LN metastasis in around 25% of cases, the SLNs were extirpated for histopathology at the time of revision surgery for the incompletely excised MCT.
Histopathology identified the parotid LN as pre-metastatic, with no evidence of metastasis in either mandibular LN. Prior cytology of the liver and spleen did not identify evidence of spread. Beetle completed a course of adjuvant lomustine chemotherapy and has been doing well since with no evidence of MCT recurrence or metastasis.
Benefits across species
As SLN mapping and biopsy is a more targeted and personalised staging approach, it significantly reduces morbidity compared to more extensive LN sampling. It also increases the detection of metastatic disease – in humans, 30% of patients benefit from additional therapies that would not have otherwise been offered. For canine MCT, as in Beetle’s case, the extirpation of metastatic LNs (and even the prophylactic removal of regional non-metastatic LNs) can improve outcome, so accurate identification of SLNs is crucial.
The Oncology Service is committed to providing the most up-to-date diagnostic and therapeutic options to improve patient quality of life and outcome and is one of few centres to offer SLN mapping via both ICTL and contrast-enhanced ultrasound.
