Transvenous PDA Occlusion
Clinical Connections – Summer 2019
Virginia Luis Fuentes and David Connolly, Professors of Veterinary Cardiology, Anne Kurosawa and Xavier Navarro Cubas, Cardiology Specialists.
Patent ductus arteriosus (PDA) is one of the most common congenital cardiac diseases in dogs. Female small breed dogs are overrepresented and a classic continuous “machinery” murmur can be auscultated at the left side of the base of the heart.
A 2D Doppler echocardiogram can be used to confirm the diagnosis.Treatment should be performed without delay as PDAs are one of the few congenital cardiac diseases that can be entirely cured. When treated early (before clinical signs), the prognosis is excellent and then the patient can have normal life expectancy and quality of life. If left untreated, most dogs with a PDA will develop congestive heart failure by one year of age.
Currently, there are two treatment options: minimally invasive transcatheter occlusion or surgical ligation. Surgical ligation in the hands of an experienced surgeon has similar success rates to transcatheter occlusion but the common reason for choosing transcatheter occlusion is the more rapid recovery time (<24 hours).
Until recently, the size of the patient was a limiting factor for transcatheter occlusion with an Amplatz canine duct occluder (ACDO), as it is placed through the femoral artery.The femoral artery of a 2-3kg dog will be too small to allow the placement of an appropriately sized ACDO. Instead, by using a transvenous approach through the jugular or femoral veins, we now offer transcatheter occlusion with a vascular occluder even in very small patients. Kayla (2.7kg Chihuahua cross) had a vascular plug placed, which successfully occluded the continuous flow across the PDA.
Her heart murmur was noted at her first vaccination and her vets suspected the presence of a patent ductus arteriosus. A referral to the RVC Small Animal Referrals was arranged to assess Kayla as a possible candidate for surgical closure or minimally invasive occlusion of her PDA. Following discussion, the owners expressed their preference for minimally invasive occlusion. The ODA was accessed by catheterising the right heart and the main pulmonary artery using fluoroscopic guidance. Her PDA was successfully occluded using the vascular duct occluder, with no residual flow.
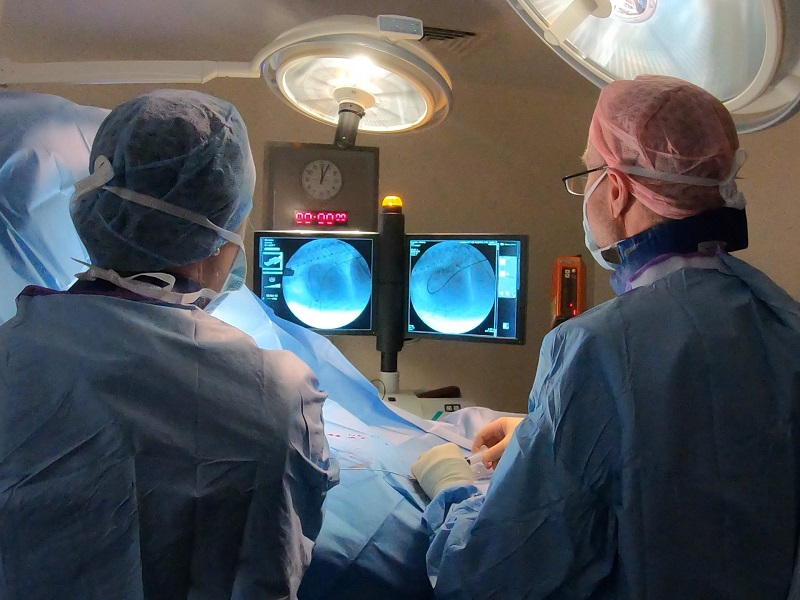
Traditionally, prior to interventional closure the PDA is outlined by invasive angiography, where an injection of angiographic contrast into a catheter in the aortic root outlines the ductus. At RVC Small Animal Referrals, transoesophageal echocardiography (TEE) and,in particular, 3D TEE plays a vital role in assessing ductal morphology prior to occlusion (Figure 1B).Transoesophageal echocardiography minimises the need for ionising radiation, reducing x-ray exposure for patients and operators as well as providing unique imaging detail.
There is always a risk of ductal rupture and death with surgical PDA closure (even though that risk is very small at the RVC), as well as a risk of incomplete closure. Interventional PDA closure has all but eliminated these risks.
