Feline Pancytopenia Update
Last updated - Monday 13th September 2021
The RVC is aware of 565 cats that are known to us based on cases treated at our own hospitals and information provided by some vets in the UK.
Of these there was 63% mortality at time of reporting.
NB. This data probably represents only a percentage of cases, as many cats may not be presented to a veterinary practice and/or investigated by a vet.
Only a small percentage of the vets in the UK are actively reporting to the RVC at this time.
The data from our survey is provided by third parties and has not been independently verified and is correct when provided by the vets concerned.
Therefore, the percentage of mortalities may change after submission of the information.
Survey for vets to log a case of feline pancytopenia →
Thursday 2 September 2021 - A spokesperson for the RVC said:
“The Royal Veterinary College (RVC) continues its investigation into the sudden increase in feline pancytopenia in cats in the UK.
“Currently, we are sadly aware of over 500 affected cats. Investigations into an underlying cause do not suggest a link with common feline infectious diseases, common toxins (e.g., heavy metals, oestrogen) or deficiencies/excesses in vitamins or minerals.
“Results of analyses by the RVC of cat food involved in the product recall published by the Food Standards Agency (FSA) have been shared with the FSA. We would like to draw your attention to the latest FSA statement published on 26 August 2021. This contains a number of Frequently Asked Questions including reaffirmation that cats should not be fed diets listed in the recall. To date the FSA’s testing and analysis has not been able to definitively determine a cause. It has not ruled out cat food or any other possible causes and its investigations are continuing.”
“Our investigations are ongoing and we are still collecting data from practising veterinarians, as well as testing food samples associated with affected and unaffected cats to determine the significance of these findings. We have shared our results with the FSA in order to assist them with their investigations into this matter.
“To support our ongoing efforts, we are encouraging vets who have seen cats with unexplained severe thrombocytopenia and/or neutropenia, with or without concurrent anaemia, to complete our survey (https://rvc.onlinesurveys.ac.uk/pancytopenia).”
What are mycotoxins?
Mycotoxins are toxic compounds that are naturally produced by different types of fungi. They can grow on a variety of different crops (e.g. grains and vegetables) before or after harvest and foodstuffs including cereals, nuts, spices, dried fruits, apple juice and coffee, often under warm and humid conditions.
Trichothecenes are a large family of chemically related mycotoxins produced by moulds like Fusarium, Trichoderma, Trichothecium and others. Type A trichothecenes include the T-2 and HT-2 toxin.
What effects do trichothecene mycotoxins have on cats?
T-2 and HT-2 toxins have a wide range of toxic effects in animals, including weight loss, loss of appetite and decreases in blood cell concentrations (white blood cells, red blood cells and platelets), leading to an increased risk for infections and/or bleeding. The European Food Safety Agency (EFSA) reports that cats are particularly sensitive to T-2 and HT-2 mycotoxins (EFSA Scientific Opinions 2011, 2017), but a lack of data hinders the establishment of a legal safe value for T-2/HT-2 concentrations in feed for cats. In some countries, a legal safe limit has been established in feeds for these mycotoxins for some species.
Further Publicly Available Resources
- COMMISSION RECOMMENDATION (EU) 2016/ 1319 - of 29 July 2016 - amending Recommendation 2006/ 576/ EC as regards deoxynivalenol, zearalenone and ochratoxin A in pet food (europa.eu)
- Scientific Opinion on the risks for animal and public health related to the presence of T-2 and HT-2 toxin in food and feed | European Food Safety Authority (europa.eu)
- Human and animal dietary exposure to T‐2 and HT‐2 toxin - - 2017 - EFSA Journal - Wiley Online Library
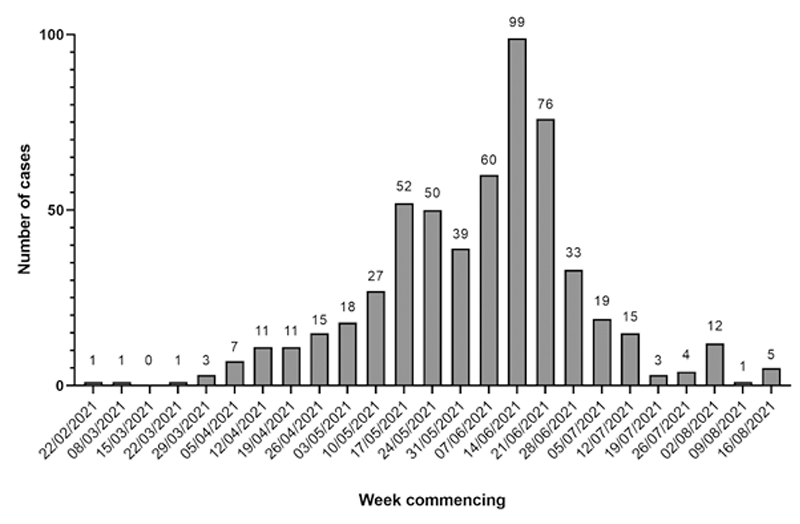
Has there been any change in number of cases reported since this problem was first noted?
Information for owners
- My cat has been eating a recalled food brand, what shall I do?
Do not feed your cat any more of this food. This is also the recommendation of the FSA who say you should follow the advice in the recall notice. Please contact the product manufacturers for brand specific questions. Further details can be found here: https://www.food.gov.uk/news-alerts/alert/fsa-prin-36-2021
You could discuss with your vet whether you would like a blood test performed looking at the levels of red and white blood cells and platelets in your cat’s blood as decreases in these levels are seen if your cat is affected with pancytopenia. - My cat is ill and I think it might have this problem, what should I do?
Please contact your vet so they can examine your cat and discuss further investigation as necessary. You may also want to contact the product manufacturers for brand specific questions if your cat has been eating one of the recalled diets. Further details can be found here: https://www.food.gov.uk/news-alerts/alert/fsa-prin-36-2021 - We are trying to gather information on all affected cats, so if your vet thinks your cat is affected then please ask them to complete our survey to allow us to learn more about this syndrome (https://rvc.onlinesurveys.ac.uk/pancytopenia). If you give your vets permission for us to contact you we may be in touch to ask you some questions, but we will not do this if you would rather not be contacted.
Information for vets
- How do I log a case:
Compete the survey at: https://rvc.onlinesurveys.ac.uk/pancytopenia - How do I recognise if a cat has this syndrome?
The clinical signs can be very vague initially (lethargy, malaise and inappetence). One of the first more specific clinical signs that can be seen is bleeding e.g. from the mouth, haematochezia, haematuria, haematemesis, melena, haematoma post blood sample. In more severe cases when bleeding is marked, patients can present collapsed with hypovolaemia. Some cats have presented with no clinical signs at all and have been diagnosed purely because another cat in the household was affected. - How do I diagnose this syndrome?
A complete blood count with blood smear examination (ideally performed at an external laboratory) is required. The cats may have a pancytopenia affecting platelets (generally <20x10⁹/l), neutropenia (generally less than 0.5x10⁹/l) and a varying level of non-regenerative anaemia depending on whether (or how much) bleeding has occurred. However it seems that earlier in the disease process only thrombocytopenia or neutropenia may be present and some (in particular very young) cats, in an apparently earlier stage of the disease, have had signs of regenerative anaemia. The pancytopenia is caused by severe generalised bone marrow hypo- to aplasia, and the gold standard method to diagnose this is bone marrow sampling (aspirate and core). - How should I treat this syndrome?
The ideal treatment for these patients is unknown. We suspect a toxic basis for the disease (though this has not been confirmed), but the toxin, and therefore any ‘antidote’ is unknown. Treatment is therefore based on supportive care. Cats should not be fed any more food which has been subjected to a recall. In unstable anaemic patients whole blood or packed red blood cells (with or without plasma) are recommended. Broad spectrum antibiosis e.g. potentiated amoxycillin is recommended for patients with a neutrophil count below 1x10⁹/l. Corticosteroid therapy is controversial. There is no evidence that it is beneficial and immunosuppressive doses may well be harmful in patients with such a low neutrophil count. Other possibly useful therapies include granulocyte colony stimulating factor (G-CSF), tranexamic acid in patients with large volume haemorrhage, cobalamin, folate and vitamin E though none of this advice is evidence based. - What should I do with a cat which seems healthy but has been eating a diet which has been re-called?
There will likely be many cats which are in this situation and in view of the FSA’s latest statement, the best approach will depend on owner finances and level of concern. Asking the owner to monitor the cat closely and to contact you if they note any of the clinical signs noted above is generally appropriate. A complete blood count (CBC) could reassure an owner or allow an asymptomatic case to be detected. We would recommend a CBC with blood smear examination (ideally performed at an external laboratory) is performed in asymptomatic cats in a household where another cat has been affected. If mild decreases in platelet, neutrophil and/or red cell numbers are noted on CBC, but levels are not compatible with those noted above, then we would recommend repeat CBC in 3-14 days depending on the severity of the decrease to monitor for progression.

